Recurrent miscarriages: causes, diagnosis and treatment
Miscarriage is a very sad experience and, if repeated, can be traumatic. Approximately 15% of pregnancies end in miscarriage before the ninth week of pregnancy.
We speak of recurrent miscarriages when there are two or more non-evolving pregnancies. In these cases, each miscarriage will increase the likelihood of recurrence in subsequent pregnancies as it indicates that there is a common cause.
Genetic alterations
Chromosomal abnormalities of the embryo are the most frequent cause of recurrent miscarriages: they account for 50-60% of cases. This percentage increases with the woman’s age. These anomalies can appear during the formation of the embryo and can be inherited from the father or the mother.
Approximately 4% of couples with recurrent miscarriages have a chromosomal abnormality in the karyotype of one of the parents. The karyotype is analysed by a blood test. It is the representation of a person’s chromosomes arranged according to their morphology and size. Each cell has 46 chromosomes, 23 pairs inherited from the mother and 23 from the father.
Chromosomal abnormalities often affect the karyotype structure: missing a piece or having an extra piece. In the carrier parent the alteration is in balance, but it can be transmitted in an unbalanced way.
The vast majority of miscarriages are due to alterations in the number of chromosomes in the embryo because the sperm and/or the egg do not have the appropriate chromosomal endowment. According to studies carried out at Institut Marquès, in the best of situations, i.e. embryos from donor sperm and eggs, almost half of them have chromosomal abnormalities. It seems a lot, but human reproduction is not very efficient.
The percentage of abnormal embryos increases with the age of the woman, with 78% of the embryos of patients in their 40s being altered.
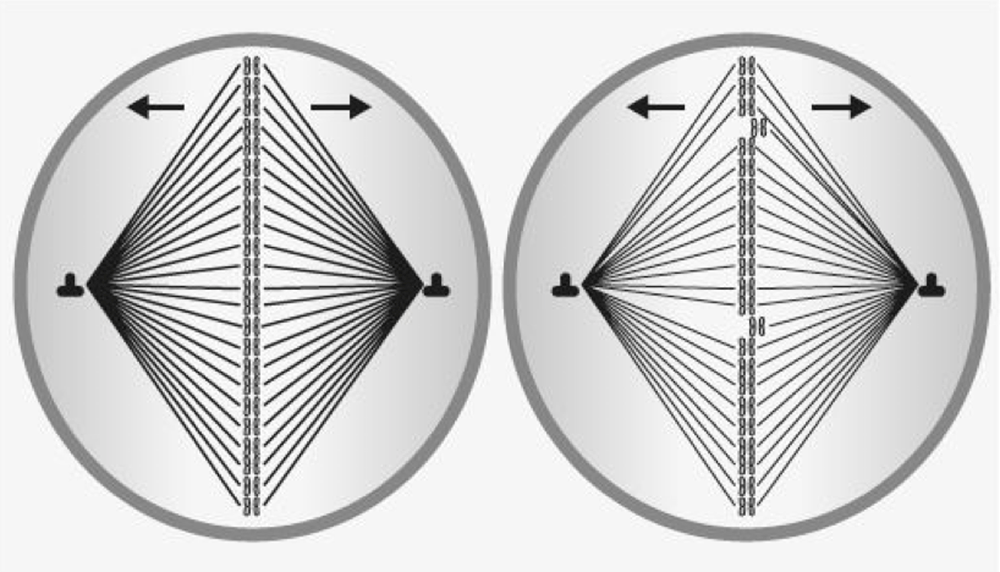
In the egg cell nucleus, after ovulation, the 46 chromosomes are placed face to face to separate. The filaments that bind them together are released, leaving 23 chromosomes. As a woman gets older, the passage of time causes alterations in this process (in young women the rods that separate them effectively are resistant. With age they become weaker and can break like the filaments of a light bulb). Therefore, there may be extra chromosomes left over (if it is 21 it will give rise to Down’s Syndrome) or less, causing fertilisation failures or embryos with genetic alterations which will mostly be early miscarriages
The risk of miscarriage for a 35-year-old woman is 20%, at 40 years of age 40%, and at 45 years of age 80%. However, ovarian age is not always the same as chronological age.
In order to know the risk of another miscarriage, we must study the patient’s ovarian reserve by analysing the anti-mullerian hormone (calculate your ovarian age by clicking on this link). To rule out that it is due to abnormalities in the chromosomal endowment of the sperm, a study in semen called FISH is recommended. Meiosis and double-stranded DNA fragmentation studies may also be adviced.
The indicated treatment for recurrent miscarriages caused by genetic alterations is In Vitro Fertilisation with Genetic Analysis of the Embryos (PGT). In this way, only chromosomally healthy embryos are transferred into the mother’s uterus.
In the case of a miscarriage, we can already determine a possible genetic cause with just a blood test.
The most common cause of miscarriage is chromosomal abnormalities in the embryo. A blood test of the patient now allows us to determine the karyotype of the non-evolving embryo within 4 days.
As soon as the embryo is implanted, embryonic DNA is found in the mother, so the analysis can be carried out following any miscarriage, even with only a week’s delay.
This is a great advance because when this study is carried out on the abortion remains, by means of curettage or chorion biopsy, there are many failures when it comes to obtaining the result and, in addition, the sample may have been contaminated with DNA from the mother.
At Institut Marquès we obtain the blood sample in our own clinic to carry out the “PregnancyLoss” analysis. The total cost is 480 euros.
- Antiphospholipid Syndrome: it occurs when the immune system mistakenly produces antibodies that increase the likelihood of blood clots. It is considered responsible for 10-15% of miscarriages. It is also called Acquired Thrombophilia.
- Autoimmune Hypothyroidism, Hashimoto’s Thyroiditis: in this disease the immune system attacks the thyroid and often prevents it from producing sufficient amounts of thyroid hormones. These hormones are related to the ovarian cycle and embryo implantation.
- Celiac disease: an autoimmune disease whose most common symptoms include chronic musculoskeletal pain, headaches, and physical and mental fatigue.
- Other immunological factors such as KIR genotype, HLA-C typing, NK cells (natural killer cells) and anti-parental antibodies have been linked to miscarriage and implantation failure but there is NO scientific evidence. Experimental studies have been carried out and it is currently considered that they should not be tested, let alone treated.
- Antiphospholipid syndrome is diagnosed by testing for anticardiolipin antibodies (ACA), lupus anticoagulant antibodies (LA) and anti-beta2-glycoprotein antibodies.
- Autoimmune Hypothyroidism presents with low T4 hormone and elevated HRT. The antibodies tested are thyroglobulin antibodies (TgAb) and thyroid peroxidase antibodies (TPO).
- Classic Coeliac Disease presents with diarrhoea, vomiting, heavy digestion and, in children, short stature and underweight. In adults, the symptoms of coeliac disease are usually different, with extra-digestive symptoms being more common. Diagnosis is completed by testing for coeliac disease antibodies.
- Antiphospholipid Syndrome requires a personalised assessment in terms of doses of acetylsalicylic acid and anticoagulants such as low molecular weight heparin. Eighty percent of patients respond to this treatment, but 20% develop Refractory Antiphospholipid Syndrome. This has a worse prognosis but, in these cases, treatment with corticosteroids is associated.
- Autoimmune hypothyroidism is treated with thyroid hormone tablets. Levels should be monitored during pregnancy as they tend to fluctuate. In patients with elevated anti-TPO and anti-TGL levels, we also recommend adding Aspirin to the thyroid hormone treatment.
- Coeliac disease is controlled by eliminating gluten-containing foods.
Hereditary thrombophilia is a genetic predisposition to increased blood clotting. It is due to genetic variants in the proteins involved in clotting. As a result, thrombi may form. They usually occur in the legs but can break off and cause pulmonary thromboembolism.
Pregnancy induces a state of hypercoagulability in all women, a physiological change to prevent haemorrhage during childbirth. In patients with thrombophilia, thrombosis may occur in the placenta, reducing vascularisation to the foetus and causing miscarriages. They are also at increased risk of postpartum thromboembolism.
The standard test for diagnosing genetic thrombophilia is a blood test for Protein C, Protein S, Antithrombin III and Leyden’s Factor V. But this test can only identify 20% of cases. The study of the genetic profile of thrombophilias allows 85% of patients with this disease to be detected.
Treatment for patients with genetic thrombophilia is carried out on an individualised basis with Low Molecular Weight Heparin.
Congenital uterine malformations in which the uterus is very small and/or deformed and others in which there is a fibrous septum that divides the uterine cavity in two “Uterus septum”. The incidence of these malformations is 0.3% in the general population and approximately 4% in patients with miscarriages.
- Double, bicornuate, unicornuate, septate and hypoplastic uteri are associated with a higher rate of miscarriage due to decreased uterine volume, abnormalities in myometrial distension and alterations in endometrial secretions due to vascularisation defects.
- T-shaped uterus. T-shaped uterus: the uterine cavity is usually triangular in shape, but in some women it is T-shaped, with a narrower, tubular cavity at the bottom.
- Fibroids inside the uterus, “submucous fibroids”, can hinder placentation and large “intramural fibroids” that deform the uterine cavity can increase the risk of miscarriage.
- Uterine synechiae. These are adhesions between the walls of the uterus. They are pathological scars that are due to sequelae of operations such as curettage, hysteroscopy for resection of fibroids, polyps or septa. There are different degrees, when they are very severe they are called “Asherman’s Syndrome”. They can hinder the growth of the endometrium and the patient may have very scanty periods or even no menstruation at all. They can cause sterility by obstructing the passage of spermatozoa or the embryo and can cause miscarriage by hindering placentation.
Alterations of the uterus are diagnosed by means of:
- Classical ultrasound, three-dimensional (3D) ultrasound allows us to see more detail.
- Hysterosalpingography HSG. It is a radiological test. It consists of injecting a contrast medium through the cervix that fills the uterine cavity and shows the shape of its internal cavity.
- Hysteroscopy. This consists of the introduction of a very fine optic through the vagina and cervix. It is connected to a video camera and allows the uterine cavity to be viewed on a screen.
- Malformations. Surgical correction of uterine malformation has not been shown to decrease the rate of miscarriage. In addition, these operations may leave scarring tissue and worsen the situation. It is only recommended in cases of a very marked septate uterus in patients with a poor obstetric history. It is not indicated to operate on T-shaped uteri.
- Fibroids. To improve the evolution of the pregnancy, it is indicated to remove “submucous” fibroids inside the uterus and large “intramural” fibroids that deform the uterine cavity. In these cases, when the woman desires a new pregnancy, embolisation of the fibroids is contraindicated.
- Synechiae. If they are mild, they are easily removed by surgical hysteroscopy. If they are important, as in Asherman’s Syndrome, the prognosis is worse, it is usually necessary to perform several surgical hysteroscopies and there is a risk of complications, of re-formation, or of not being able to free the entire uterine cavity.
Misconceptions about recurrent miscarriages
Hormonal disorders
Thyroid disorders and diabetes, if medically controlled, are NOT a cause of miscarriage. Nor is there scientific evidence that hyperprolactinaemia or corpus luteum insufficiency are.
Other causes and recurrent miscarriages with unknown cause
Infections such as listeriosis in the first trimester of pregnancy can cause termination of pregnancy but infections are NOT a cause of recurrent miscarriage.
- Intense stress affects the regulation of cortisol and catecholamines and can reduce the oxygen supply to the foetus inducing foetal growth retardation but are NOT a cause of miscarriage.
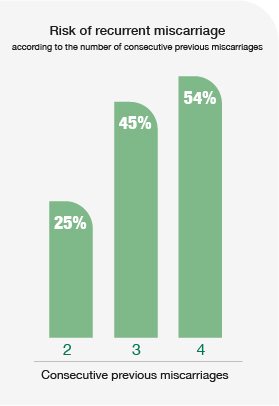
In many patients who have had miscarriages, we do not know the cause even if diagnostic tests are done. There is still a lot of research to be done in this respect but the important thing is to know if it will happen again. According to the literature, the risk of miscarriage is 25% with 2 previous consecutive miscarriages, 45% with 3 previous consecutive miscarriages and 54% with 4 previous consecutive miscarriages. This is at the level of general statistics but there are causes that increase or decrease this risk: it is higher if antiphospholipid syndrome is diagnosed and it is lower if it is assumed that they were due to advanced maternal age and the next pregnancy occurs with transfer of a chromosomally analysed embryo.
In the last 10 years, we have made enormous progress in the diagnosis of repeat miscarriages of embryonic origin. The great challenge lies in improving the diagnosis of recurrent miscarriage of maternal origin. This remains our main research goal. The fact that in many cases the cause is unknown and the subsequent pregnancy develops normally has led to all kinds of diagnoses and treatments.

Assisted Reproduction Doctor of the Year 2019
The opinion of Dr. Marisa López-Teijón
I am concerned about what is happening in my speciality with the management of recurrent miscarriages and embryo implantation failures in IVF. Since we still do not know a lot of things, it has become fashionable to do all kinds of unscientific diagnostic tests and treatments worthy of shamanism. Read more